
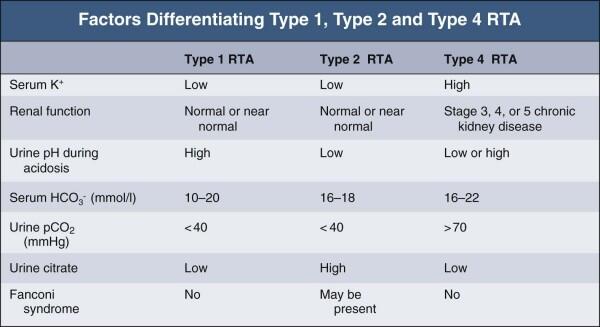
Aldosterone resistance (nl to high aldosterone, nl to high cortisol). Selective aldosterone deficiency (low aldosterone, normal cortisol). Adrenal insufficiency, Addison's (low aldosterone, low cortisol). Serum aldosterone and cortisol levels to determine between:. 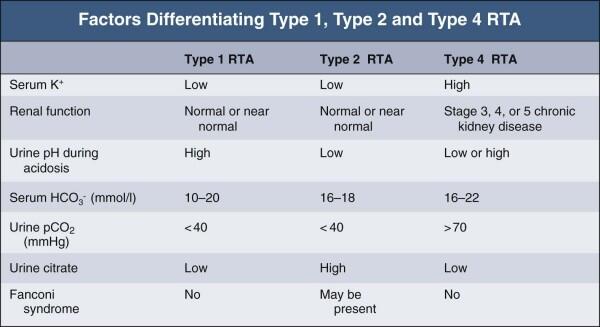
Three new models have been added to the IHI-Sulzer RTA range of engines these are the RTA84M.
Mild acidosis, with bicarb generally > 17 mEq/L THE TRENDS OF THE IHI-SULZER RTA TYPE MARINE DIESEL ENGINE. Nephrolithiasis, calcium stones from chronic acidosis causing bone resorption and hypercalciuria. Urinary anion gap > 50 mEq/L = Na + K - Cl This type is caused by impaired distal acidification and is characterized by the inability to lower urinary pH maximally (. Normokalemia may be seen in chronic interstitial renal disease. Type I RTA - impaired H+ and ammonium secretion. Treat adults with bicarb 5.5 if undergoing alkali therapy. May require IV bicarbonate for severe acidosis. Generally, 5-15 mEq/kg/day oral bicarbonate. For type I and II RTA, treat all children and infants. Children should be treated due to impaired growth. It consists of a few Driving licence test questions. RTA TYPE DRIVERS
To get your Drivers licence, you would need to pass Dubai driving theory test. A Drivers licence gives you practical experience to legally drive vehicles (car, motorcycle, etc) in Dubai.
Mild acidosis in adults with bicarb > 20 mEq/L may not require treatment The Roads and Transport Authority of UAE (Dubai) conducts the RTA Theory Test to issue Driving Licence. Note that when hyperkalemia is present, aldosterone should be elevated, so a "normal" aldosterone level may be relatively low. Plasma aldosterone and cortisol for type IV RTA. Diabetic nephropathy (hyporenin/hypoaldosteronism). Familial (decreased H+/K+-ATPase, Na+/K+-ATPase activity). 
The principal buffers in the urine are ammonia and phosphate (titratable acid). Inherited type 3 RTA is caused by mutations of CA II (chromosome 8q22) resulting in carbonic anhydrase II deficiency.
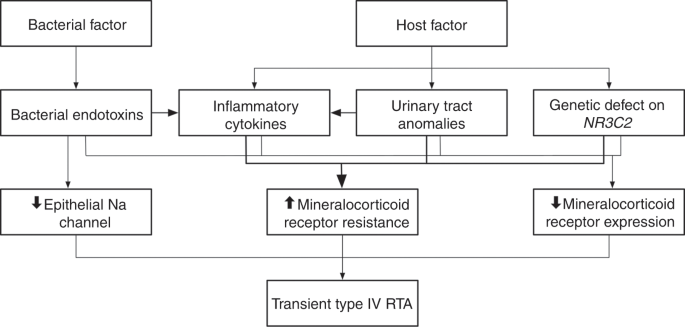
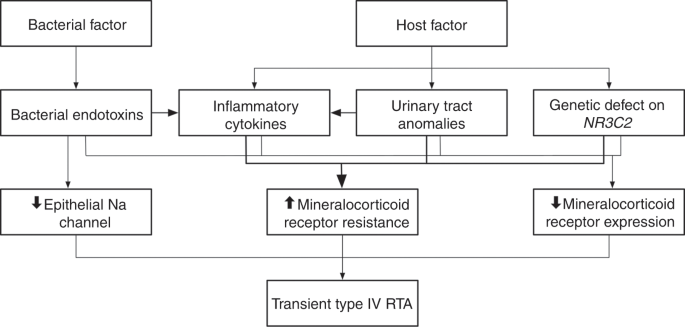
Drugs - Lithium, amphotericin B, ifosfamide Type 3 is a vanishingly rare combination of types 1 and 2. Primary metabolic (cystinosis, von Gierke's). Vitamin D deficiency, rickets, hypophosphatemia. Heavy metals ( Lead, mercury, copper/ Wilson's). Differentiate from uremia in which acidosis is anion gap. Diagnostic classification starts with low, normal, or high serum potassium. Distal RTA results from the failure of net renal acid excretion, usually due to an inability to excrete H + ions into. All forms of renal tubular disorders are characterized by hyperchloremic metabolic acidosis. Causes hyperchloremic metabolic acidosis, non-anion gap Distal renal tubular acidosis (dRTA) is the classic form of renal tubular acidosis, which is also called renal tubular acidosis type 1. Class of disorders characterized by impaired reabsorption of filtered bicarbonate or excretion of hydrogen ions. The roles of mineralocorticoid deficiency and hyperkalemia in the pathogenesis of type IV RTA will be considered and the ameliorative effects of treatment with fludrocortisone, furosemide, and dietary potassium restriction reviewed. Many patients with type IV RTA, but not all, have hyporeninemic hypoaldosteronism. Because we receive certain types of information from visitors to the RTA website, we want you to understand the terms and conditions regarding the use of. It is frequent among hospitalized patients as it is related to type 2 diabetes mellitus (T2DM) and common medications such as ACE-inhibitors (ACE-is) and trimethoprim-sulfamethoxazole (TMP-SMX). The pathophysiologic characteristics include: reduced renal clearance of potassium a reduced rate of renal bicarbonate reabsorption at normal plasma bicarbonate concentrations (the magnitude of which is insufficiently great to implicate the proximal tubule) an unimpaired ability to maintain a steep hydrogen ion concentration gradient between blood and urine during acidosis and a reduced rate of renal net acid excretion despite highly acidic urine, due in part to reduced urinary excretion of ammonium, which in turn appears to be due in part to suppression of renal ammoniagenesis by hyperkalemia. Type IV renal tubular acidosis (RTA) is the only RTA characterized by hyperkalemia, and it is caused by a true aldosterone deficiency or renal tubular aldosterone hyporesponsiveness. Type IV renal tubular acidosis (RTA) is a syndrome of tubular dysfunction manifested clinically by persisting hyperkalemia and metabolic acidosis that occurs usually in patients with mild to moderate chronic glomerular insufficiency.





 0 kommentar(er)
0 kommentar(er)
